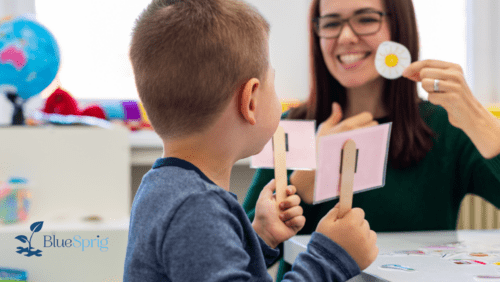
As a caregiver of a child on the autism spectrum, you need a partner that you can count on. We provide collaborative ABA therapy that focuses on support and guidance for all members of your family. Our team is available to consult with other health and education professionals involved in your child’s care. BlueSprig is here to make sure you never feel like you are on your own. We have dedicated teams that work to build relationships with local and national resources to better support your family throughout the entire journey.